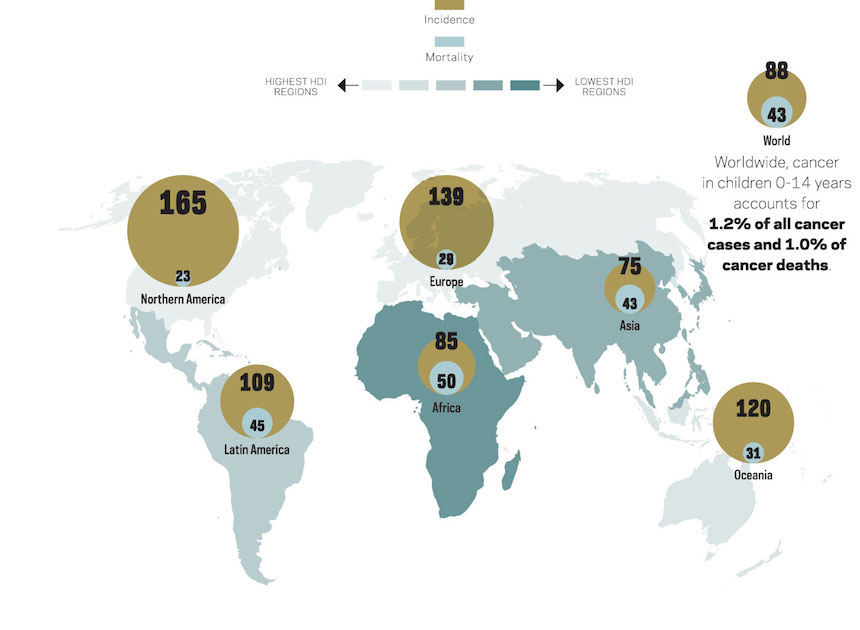
World Cancer Day is celebrated globally on February 4 under the tag line “We Can. I Can”. Increased awareness and education about childhood cancers means that more lives are saved. The Conversation Africa’s Health and Medicine Editor Joy Wanja Muraya spoke to Jessie Githanga on the challenges of diagnosing and treating childhood cancer in Kenya.
What are the top cancers in Kenya, regionally and in Africa? What are the most likely causes?
In Kenya, accurate data about the most common forms of cancer is unavailable because the country doesn’t have an updated population based cancer registry. It therefore has to rely on regional registries that are largely hospital based. Though not comprehensive, it’s nevertheless still useful as most patients with cancer will eventually go to a hospital where data will be collected.
The top childhood cancers are lymphoma (a form of cancer affecting the immune system), cancers of the blood (leukaemia), brain, eye, kidney and muscle cells.
Regional differences in the top cancers is seen in countries like Mozambique, Uganda, Zambia and Malawi where childhood HIV/AIDS is more common. This leads to AIDS related cancers like Kaposi’s sarcoma (a cancer of the blood vessels) and certain types of lymphoma.
In countries with high rates of malaria infection, Burkitt’s lymphoma is the most common childhood cancer. It’s less common in the developed world where signs and symptoms differ.
Are childhood cancers different from adult cancers?
They differ in two ways.
Adult cancers are strongly associated with lifestyle related risk factors like unhealthy eating, being overweight and obesity, lack of exercise as well as increased tobacco and alcohol use.
Are children in Africa receiving appropriate treatment? What are the challenges on the continent?
In developed countries a child diagnosed with cancer has an 80% chance or more of surviving whereas the survival rate of children in Africa is less than 20%.
The causes are many and interrelated. One is late diagnosis due to lack of awareness of cancer in children among guardians, health care workers and the general population coupled with poor access to treatment facilities.
There’s also inadequate diagnostic capability and a disturbing paucity of treatment facilities especially those designed for childhood cancer in most sub Saharan African countries.
The prohibitive cost of chemotherapy drugs, few radiotherapy facilities as well as a lack of bone marrow transplantation technology, compounds the problem making treatment expensive.
The problem of insufficient health care workers trained in paediatric cancer, especially oncologists, pathologists, surgeons, nurses, pharmacists and palliative care experts needs urgent attention.
Treatment protocols are rarely standardised, evidence based or adapted for each developing country’s capacity. There’s little research into local childhood cancers and especially clinical trials . This is a sorry state of affairs given that the best treatments in cancer are often in the context of a clinical trial.
Current evidence shows that even where the types of cancer may be similar to those in developed countries there are biological differences that have a significant impact on the treatment choices and outcomes.
It’s therefore imperative that further research including clinical trials to identify suitable treatments are done to improve treatment outcomes.
What is Kenya doing about the gaps?
Kenya has now woken up to the fact that cancer is a serious problem. Even though most attention has been given to the common adult cancers, such as those of the male and female reproductive tracts (breast, cervical and prostatic cancers), more attention is now being paid to childhood cancers through efforts of the government, Non-Governmental Organisations, professional bodies and civil society.
Some of these initiatives include the collaborative efforts by the Ministry of Health and the National Cancer Institute in the US, Kenya Network of Cancer Organisations , Kenya Hospices and Palliative Care Association, Kenya Society for Haematology and Oncology and various independent donors and well-wishers.
Groups specifically targeting children have been set up, like the Kenya Childhood Cancer Trust and Hope for Cancer Kids. Health care financing for all aspects of treatment of childhood cancers are now being considered by the National Health Insurance Fund.
Studies in public hospitals have shown that children with cancer who have health insurance funding have better chances of survival than those who don’t. While there’s still much to be done, these efforts will yield fruit with time. More coordination of the various stakeholders needs to be made to avoid duplication of efforts.
What is the way forward for Africa in dealing with cancer?
Advocacy and creating public awareness are key points if Africa is to move towards tackling childhood cancers.
Holding international and national cancer awareness days should be coupled with continuous awareness efforts.
Twinning programmes linking centres in resource-rich countries with those in resource-limited ones have worked well in Ethiopia and Ghana to improve capacity and patient survival.
Clinical trials that can improve survival as well as enhance capacity need to be performed.
The International Society for Paediatric Oncology offers training information. Training can be more cheaply offered in other African countries with established training programmes including South Africa, Egypt and Ethiopia. Twinning could also help less well established programmes in other African countries.
![]()
Jessie N. Githanga, Prof, Haematology and blood transfusion, University of Nairobi
This article was originally published on The Conversation. Read the original article.